Over One Third of Lower-income Latino Adults Living with Children Have Frequent Anxiety or Depressive Symptoms, and Most Do Not Receive Mental Health Services
Jul 19, 2022
Research Publication
Over One Third of Lower-income Latino Adults Living with Children Have Frequent Anxiety or Depressive Symptoms, and Most Do Not Receive Mental Health Services
Author
This data snapshot is part of a series documenting how Latino children, families, and households have been faring since the onset of the COVID-19 pandemic. Each snapshot draws from the latest publicly available data sources to examine a specific domain of child and family well-being and provide a brief overview of social and policy context relevant to the findings. Recent snapshots have focused on child care disruptions, poverty, housing insecurity, food insufficiency, and multiple hardships experienced by Latino households with children.
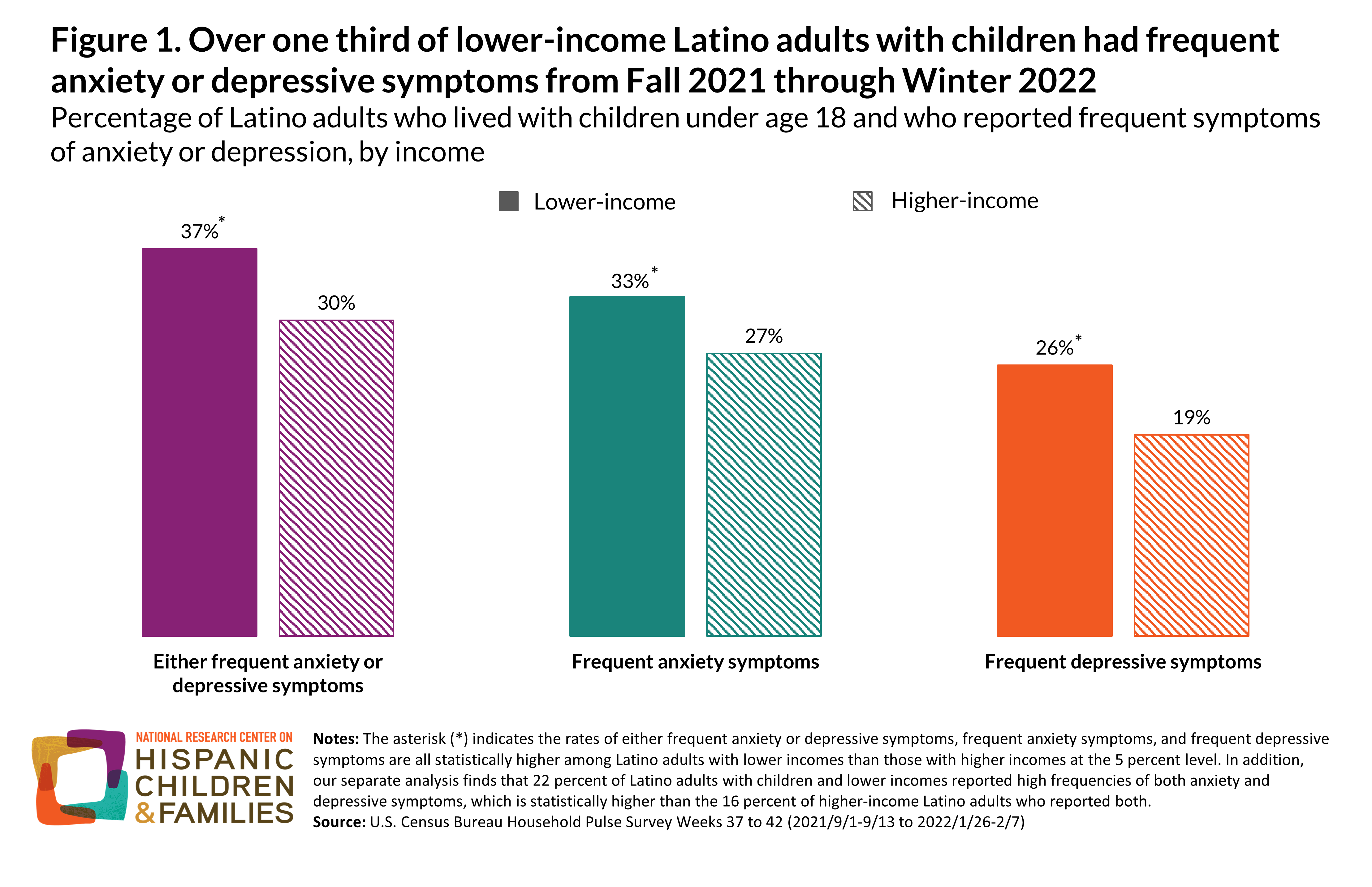
Many Latino families with children have experienced multiple hardships during the COVID-19 pandemic, including employment loss, housing and food insecurity, disrupted schools and child care, and worsened health—especially those families with low incomes. Although economic conditions have since improved for many Latino adults and their children, our analysis of the latest data shows that 37 percent of Latino adults with lower incomes (defined here as less than 200% of the federal poverty line) and living with children reported frequent anxiety or depressive symptoms this past fall and winter (September 2021-February 2022). This includes 33 percent of Latino adults who reported frequent anxiety symptoms, 26 percent who reported frequent depressive symptoms, and 22 percent who reported both; these rates are statistically higher than seen among their higher-income Latino peers. While not reflective of clinical diagnoses, these reported symptoms—when occurring at high frequencies—signal possible cases of an anxiety or depressive disorder, according to the screening instruments that ask about these symptoms (Generalized Anxiety Disorder 2-item and Patient Health Questionnaire 2-item).
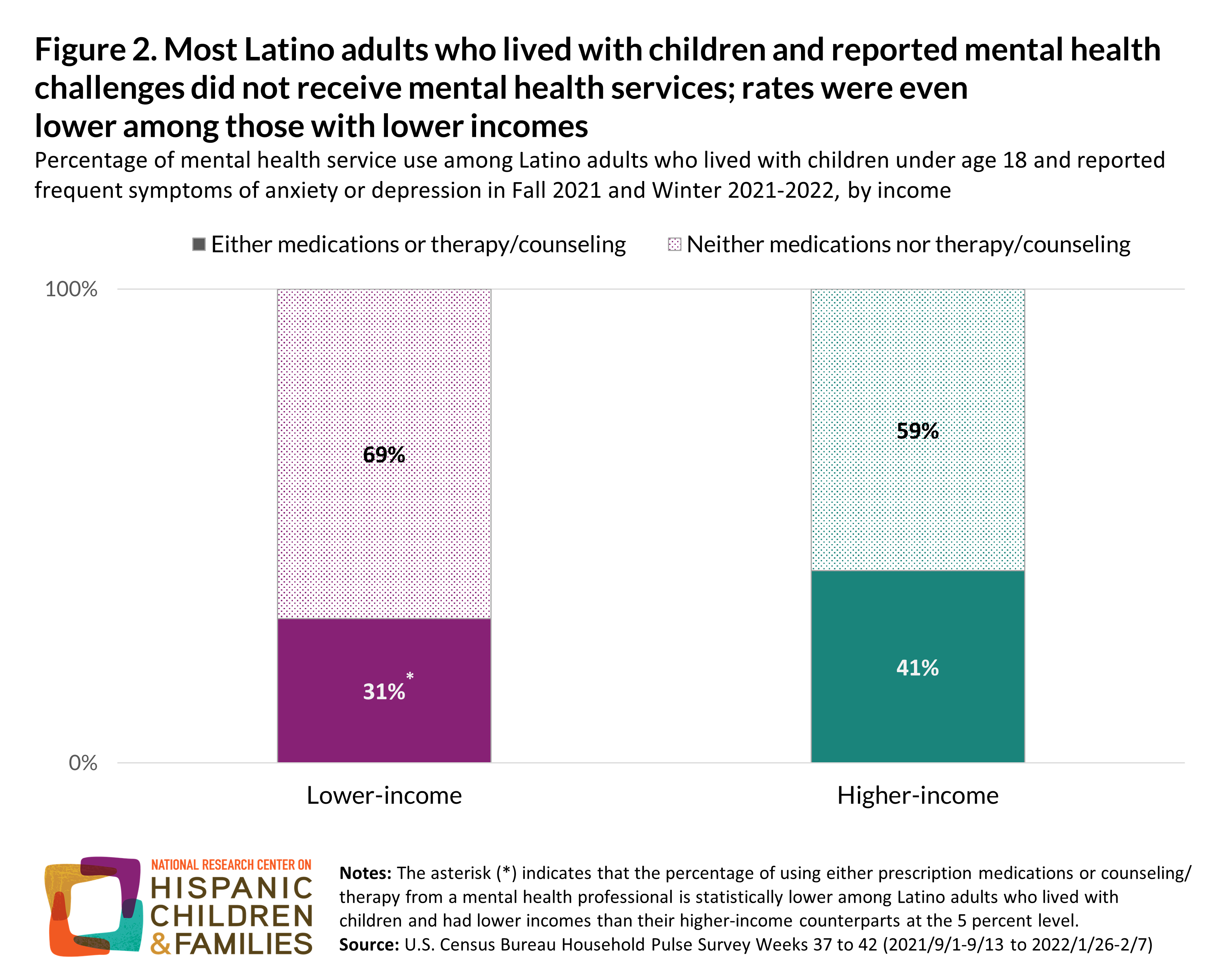
Mental health issues can be especially difficult when individuals have limited access to mental health services or face high barriers to using these services. Regardless of income status, most Latino adults with either frequent anxiety or depressive symptoms did not report using mental health care. These adults neither received mental health counseling or therapy from a mental health professional nor took prescription medications to address their mental health needs. However, this unmet need is higher among those with lower incomes: 31 percent of lower-income Latino adults with children who reported frequent depressive or anxiety symptoms received either type of mental health care, compared to 41 percent of their higher-income peers. When left unaddressed, Latino adults’ mental health conditions can have important implications for the children who live with them and for whom they are likely to care.
Addressing Barriers to Receiving Services Can Improve the Mental Health of Lower-Income Latino Caregivers
Caregivers’ mental health has a unique contribution to the health and developmental well-being of their children. Reducing caregivers’ psychological distress can promote children’s developmental, behavioral, and physical health through improved parent-child interactions and family relationships. Addressing poverty and material hardships that aggravate caregiver stress can increase positive parenting behaviors and reduce the risk of anxiety and depression. Given the pandemic’s disproportionate economic impact on Latino families, mental health care can mitigate caregiver stress and prevent further mental health challenges. However, Latino families are less likely than their non-Hispanic counterparts to receive mental health care, especially among families with low incomes.
Underutilization of mental health care among low-income Latino individuals can be traced to a combination of structural and cultural factors. First, lack of health insurance and paid sick leave, relatively low earnings, the high cost of mental health care, and immigration-related issues all present challenges in accessing mental health services among Latino persons. Implicit bias against Latino and dark-skinned individuals, shortages of mental health professionals in low-income Latino communities, and limited availability of mental health care in Spanish also present barriers to accessing mental health services in the Latino community. These factors are further compounded by individual and cultural factors such as stigma around mental health problems and services use and lack of knowledge of treatment or awareness of mental health need. Addressing structural barriers to mental health care and improving access to culturally responsive mental health care is imperative to improve mental health service use and mental health conditions among Latino families, particularly those with low incomes.
Methodology
We analyzed data from the Household Pulse Survey, which is the Census Bureau initiative to collect timely information on the economic and health-related well-being of individuals and households during the COVID-19 pandemic. We limited our sample to adults who self-identified as being of Latino or Hispanic origin and who lived with a child (or children) under age 18 during biweekly data collection periods from 9/1/2021-9/13/2021 to 12/6/2021-2/7/2022 (referred to as weeks 37 to 42 by the Census Bureau or as Fall 2021 to Winter 2021-2022 in this snapshot). We combined data from these months since rates of mental health symptoms remained largely unchanged during the fall and winter months and because combining data allowed us to increase the power of subgroup analyses by income. We applied person weights provided by the Census Bureau to all estimates and statistical tests shown. We began with a sample of 16,801 Latino adults with children in the analytic period, eliminated 3,460 observations with missing data on mental health conditions or utilization, and then removed another 1,736 observations with missing reports of income. A disproportionate share of those with missing data on mental health or income had a high school degree or less. Because mental health utilization was less common among less-educated adults than among their peers (based on our analysis of non-missing data), we may have underestimated unmet need among those with mental health needs. Our exclusion criteria left a final sample of 11,605 Latino adults with children. About 66 percent (weighted) of these adults lived in households with low incomes (or below 200% of the federal poverty level).
Our anxiety and depression measures are based on the two mental health instruments that the Survey administers: Generalized Anxiety Disorder 2-item (GAD-2) and Patient Health Questionnaire-2 (PHQ-2). GAD-2 uses two questions to ask respondents how often, over the last two weeks, they have been bothered by (1) feeling nervous, anxious, or on edge; and (2) not being able to stop or control worrying. PHQ-2 asks how often respondents have been bothered, also over the last two weeks, by (1) having little interest or pleasure in doing things; and (2) feeling down, depressed, or hopeless. In both assessments, respondents are given four choices: not at all (scoring 0), several days (scoring 1), more than half the days (scoring 2), and nearly every day (scoring 3). Following the scoring rubric, for each instrument, we summed the scores across the two items and considered persons who scored 3 and above to have had frequent anxiety or depressive symptoms. Clinically, this level of scoring identifies a possible case of generalized anxiety disorder and major depression, respectively, and suggests that a further diagnostic evaluation is warranted.
Following the questions on mental health symptoms, the Survey inquires whether—at any time in the last four weeks—the respondent (1) took prescription medication to help with any emotional issues, concentration, behavior, or mental health; and (2) received counseling or therapy from a mental health professional such as a psychiatrist, psychologist, psychiatric nurse, or clinical social worker. We treated any affirmative response to either of these questions as indicative of any utilization of mental health care, services, or interventions. Because the reference periods are different between the questions on mental health symptoms and on interventions, we acknowledge the limitation that one event might precede the other (and vice versa). Finally, using data on pre-tax household income from 2020, we constructed the low-income indicator that flags individuals with income levels roughly below 200 percent of the federal poverty level as those with “low incomes.” See also the technical appendix of this data point.
| Title | Study period | Data source | Analysis |
|---|---|---|---|
| Rates of anxiety and depression symptoms declined in 2021, remained higher than pre-pandemic | January 2021 to December 2021 | U.S. Census Bureau’s Household Pulse Survey | Prevalence of anxiety or depression by month, age, race/ethnicity, sex, education, income, state |
| Estimated prevalence of and factors associated with clinically significant anxiety and depression among US adults during the first year of the COVID-19 pandemic | 2020 compared with 2017 to 2019 | U.S. Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System (BRFSS) | Multivariate analysis of factors associated anxiety and depression |
| Young adult anxiety or depressive symptoms and mental health service utilization during the COVID-19 pandemic | June to July 2021 | U.S. Census Bureau’s Household Pulse Survey | Anxiety/depressive symptoms, mental health care utilization, and unmet counseling/therapy needs among young adults |
| Vaccinated adults report symptoms of anxiety or depression less frequently than the unvaccinated | January 2021 to December 2021 | U.S. Census Bureau’s Household Pulse Survey | Prevalence of anxiety or depressive symptoms by place of work, frontline sector, and vaccination status |
| COVID-19 pandemic and mental health problems of adults in United States: mediating roles of cognitive concerns and behavioral changes | August 2020 to December 2020 | U.S. Census Bureau’s Household Pulse Survey | Multivariate analysis of factors associated anxiety and depression |
| Racial and ethnic disparities in mental health and mental health care | April 2020 to January, 2021 | U.S. Census Bureau’s Household Pulse Survey | Predicated probabilities of depression/anxiety and mental health care use by race/ethnicity |
| State health facts | April 2020 to March 2022 | U.S. Census Bureau’s Household Pulse Survey | Mental health symptoms, total and by state |
| Symptoms of anxiety/depressive disorder during COVID | August 2021 to February 2021 | U.S. Census Bureau’s Household Pulse Survey | Mental health symptoms, mental health care use, unmet need by race/ethnicity |
| COVID coincided with elevated anxiety and depression symptoms | April 2020 to December 2020 | U.S. Census Bureau’s Household Pulse Survey | Mental health symptoms, by age, race/ethnicity, gender, education level, household income, employment status, and by state |
| National and state trends in anxiety and depression severity scores among adults during the COVID-19 pandemic – United States, 2020-2021 | August 2020 to June 2021 | U.S. Census Bureau’s Household Pulse Survey | State-specific trends in anxiety and depression severity scores and correlates |
| Trends in psychological distress and COVID-19 incidence across 15 U.S. metropolitan statistical areas in 2020 | April 2020 to December | U.S. Census Bureau’s Household Pulse Survey | Trends in anxiety or depression and COVID cases |
| The impact of the COVID-19 vaccine distribution on mental health outcomes | April 2020 to May 2021 | U.S. Census Bureau’s Household Pulse Survey | Multivariate analysis of COVID vaccination availability and anxiety or depression systems |
| Beyond the case count | September 2020 | Commonwealth Fund International Health Policy COVID-19 Supplement Survey, 2020 | COVID-related mental health conditions by gender, income, and race/ethnicity |
| COVID-19, economic pressure, and Americans’ mental health | September 2020 | U.S. Census Bureau’s Household Pulse Survey | Anxiety or depression by age, race/ethnicity, state |
| Hispanic American mental health disparities report | February 2021 | U.S. Census Bureau’s Household Pulse Survey | Unmet need for mental health care among Latinx by state |
Suggested Citation:
Chen, Y., & Ramos-Olazagasti, M. A. (2022). Over one third of lower-income Latino adults living with children have frequent anxiety or depressive symptoms, and most do not receive mental health services. National Research Center on Hispanic Children & Families. https://doi.org/10.59377/244k3083b
Copyright 2025 by the National Research Center on Hispanic Children & Families.
This website is supported by Grant Number 90PH0032 from the Office of Planning, Research & Evaluation within the Administration for Children and Families, a division of the U.S. Department of Health and Human Services totaling $7.84 million with 99 percentage funded by ACF/HHS and 1 percentage funded by non-government sources. Neither the Administration for Children and Families nor any of its components operate, control, are responsible for, or necessarily endorse this website (including, without limitation, its content, technical infrastructure, and policies, and any services or tools provided). The opinions, findings, conclusions, and recommendations expressed are those of the author(s) and do not necessarily reflect the views of the Administration for Children and Families and the Office of Planning, Research & Evaluation.